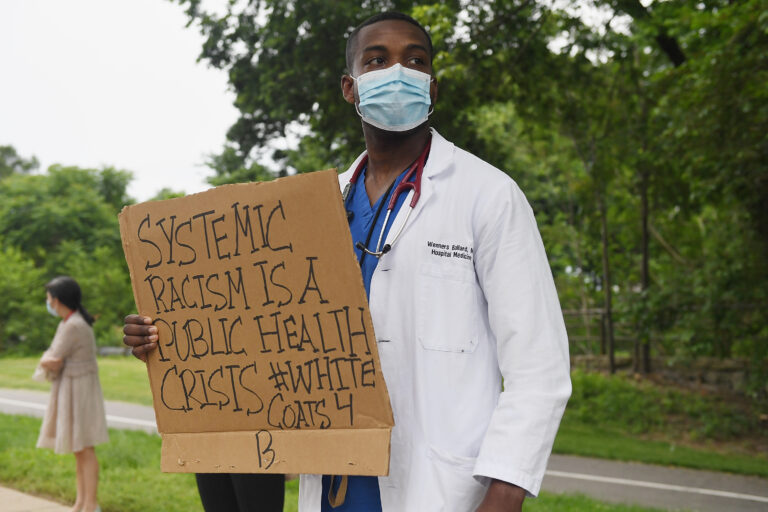
Why medical racism is still a problem
There is no surprise that Black people do not receive the same level of healthcare as their white counterparts, which increases their mortality rates and lowers their quality of life. What is even worse is that major hospital networks across the country, including Kaiser Permanente, Cleveland Clinic, Mayo Clinic, and Johns Hopkins Hospital, continue to use race norming in their eGFR (a measure of kidney health) testing algorithms, despite years of criticism from experts on the dangers of using race as a proxy for kidney health.1 In medical treatment and testing, “race norming,” or using race as a factor, has been documented for years. This practice is called race norming because it normalizes — or lowers — the standards of care for Black patients.2 Many times those tests have misdiagnosed Black patients as not having kidney disease at all when in fact, they had it, leaving them off of lifesaving kidney transplant lists or incurring expensive medical bills because their condition was not detected until it progressed to a more severe stage.
We must push hospitals to adopt fair testing practices that do not disproportionately target Black people.
Race norming tests for kidney health is a problem in and of itself, but what makes it particularly heinous is that Black patients are discriminated against more than any other group. Anti-Blackness is systemic. Anti-Blackness tells us that harm perpetrated against Black bodies isn’t violence because Black people (or animals) deserve whatever they get; there are no real consequences to be had. Anti-Blackness is an existential threat to humanity; without it, society couldn’t function because equality would be embraced as normalcy instead of something unattainable.
When a misdiagnosis occurs, it can have serious and unnecessary consequences for everyone. Both the economy and patient productivity suffer, not to mention how healthcare resources are utilized. Overwhelming medical bills harm families and communities. We also might see an uptick of lawsuits as we did with the NFL.3 Black people are subject to greater chances of being misdiagnosed with kidney failure or, conversely, having an inaccurate diagnosis. Black people account for approximately 1 out of 9 cases of diabetes, so inequities must be addressed immediately to prevent further tragedies.
All clinicians must be trained not to consider race when calculating an individual’s eGFR. The medical community needs to right historical wrongs against marginalized groups. In medical school, many medical professionals are presented with misguided information. Further, assigning a medical diagnosis to genetics or race alone ignores social determinants of health4, a more proactive approach to treating kidney disease among Black patients. Medical schools are not doing enough to ensure that students are aware of racism in medicine must continue to address racism head-on through courses on social determinants of health and implicit bias.5
Kaiser Permanente, Cleveland Clinic, Mayo Clinic, Johns Hopkins Hospital, the Association of American Medical Colleges, and other healthcare providers must take action against race norming immediately. Holding the healthcare community accountable requires demands that outline the changes we want to see, and propose the solutions that will help us get there. Changing healthcare policy systematically is the only way to achieve justice.
1. Inserro, Allison. “Flawed Racial Assumptions in EGFR Have Care Implications in CKD.” AJMC, AJMC, 19 Dec. 2020, https://www.ajmc.com/view/flawed-racial-assumptions-in-egfr-have-care-implications.
2. Canada, Tracie. “The NFL’s Racist ‘Race Norming’ Is an Afterlife of Slavery.” Scientific American, Scientific American, 8 July 2021, https://www.scientificamerican.com/article/the-nfls-racist-race-norming-is-an-afterlife-of-slavery/.
3.“The NFL’s Reversal on ‘Race Norming’ Reveals How Pervasive Medical Racism Remains.” NBCNews.com, NBCUniversal News Group, 8 June 2021, https://www.nbcnews.com/think/opinion/nfl-s-reversal-race-norming-reveals-how-pervasive-medical-racism-ncna1269992.
4.“Social Determinants of Health.” Social Determinants of Health — Healthy People 2030, https://health.gov/healthypeople/objectives-and-data/social-determinants-health.
5. Weiner, Stacy. “Medical Schools Overhaul Curricula to Fight Inequities.” AAMC, 25 May 2021, https://www.aamc.org/news-insights/medical-schools-overhaul-curricula-fight-inequities.